COVID-19 is a global and national media star unlike any we have seen in our lifetimes. Headlines in all of the newsprint media, sole subject for the radio talk programs, swamping the internet, and a subject fascinating enough to even make Wolf Blitzer seem interesting. COVID-19 has even eclipsed the news bulletins from the NFL scouting combine in America’s attention span.
The difficulty for most of America is that COVID-19 is primarily a science problem. Of course, the epidemic has impacted the political systems and economies of every nation and the damage is only beginning to be felt. Nevertheless, this outbreak, the virus itself, the public health interventions, the modeling and projections, and the health care preparations all fundamentally derive from the science of epidemiology – my field. Do you have any idea how strange it is for epidemiologists to have the entire country using terms like epi curve, pandemic, and interventions? It is positively surreal and, to be honest, I wish it wasn’t happening.
With all of the epidemiology jargon being bandied about, it occurred to me that i might be able to help with a quick primer of many of the terms that the media and scientists are using on a daily basis. I will try to be concise and practical. See if it helps.
EPIDEMIOLOGIC CURVE (EPI CURVE)
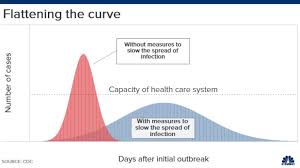
We’ve all heard a lot lately about “flattening the curve”. Delaying and reducing the rise of the in the curve of this virus is critical to limiting the damage that COVID-19 may wreak on our health care system and society as a whole.
For any type of disease outbreak, one of the first acts of an investigator is to plot the incidence of cases over time – an epi curve. Epi curves convey a wealth of information to a trained investigator, the discussion of which is beyond the scope of this essay, but suffice to say the the epi curve will be followed closely by public health authorities throughout this pandemic. For an infection like this virus, the epi curve (see image above) might begin with a relatively shallow slope as the first cases begin to show, but as more and more infected people contact the un-immunized population, the incidence rate will result in a steep slope upward representing a large number of cases over a short period of time. Once the peak is reached, the incidence rate will remain elevated for a period of time and only begin to fall when the recovered people represent a significant proportion of the population, reducing the infection rate. Public health interventions are designed to delay that rapid increase and to actually reduce the overall number of cases, therefore “flattening the curve”. If we are unsuccessful at this reduction and delay, patients will die in the US due to a lack of equipment and a paucity of skilled medical staff. For most of us, an untenable outcome.
NONPHARMACEUTICAL INTREVENTIONS (NPIs)
When a novel virus arises and suddenly spreads around the globe, no vaccine is readily available to protect the population. Since neither antibiotics nor any other pharmaceutical treatments are particularly effective against viruses, public health authorities rely on nonpharmaceutical interventions (NPIs) to fight the pandemic and protect the population. Some of these NPIS have been in play since the 1918 Spanish flu pandemic while others have been developed more recently.
I will highlight a few of the most discussed NPIs below, but I want to make clear that the effectiveness of these interventions in limiting the havoc that COVID-19 is poised to cause in this country depends heavily on the community’s acceptance and participation. Political and public health leaders MUST convey a strong and logical case to the public not only of the danger of the threat, but also of the effectiveness of these actions in reducing that threat.
Here are a few of the NPIs that the US population, and much of the world, has been encouraged to follow.
Hand Hygiene and Respiratory Etiquette – Frequently and thoroughly wash your hands and cover coughs and sneezes. Pretty self-explanatory, right? Protects yourself and the community.
Home Isolation and Home Quarantine – These terms are often used interchangeably, but they actually have different meanings. Isolation refers to ill people remaining in their homes or in an isolation room of a hospital. Home quarantine focuses on family members of ill patients or those people thought to have come into contact with a COVID-19 case remaining in their homes for the incubation period of the infection. Both of these interventions are designed to reduce the spread of disease from contaminated individuals or people who might be contaminated.
Social Distancing – This intervention differs substantially from the ones above because it is targeted at people who have not yet been connected to the disease in any way. Social distancing (SD) is a series of strategies designed to reduce face-to-face contact among members of a population, thereby reducing person-to-person transmission. SD measures can be put into place in a workplace, retail setting, school, medical care facility, or even the general population. One metric of the seriousness of a viral outbreak is the extent of SD that is put into play.
Closing schools, postponing mass gatherings, and shuttering restaurants are all interventions that can be imposed to reduce transmission, but only in the most dire circumstance. Ordering vast swaths of the population in geographical areas to stay in their homes and, effectively, “shelter in place” is a draconian intervention that conveys, as words cannot, the seriousness of our situation. These orders have now been given in at least 4 states with more to come.
So, those are some of the terms being used daily by members of the press and the scientific community. Now is an opportunity to take a quick look at where we stand.
A novel respiratory virus infected a human in China sometime in late 2019. With no immunity in any population, the virus spread quickly throughout Hunan Province and was quickly an epidemic. In most people , the virus caused a relatively mild respiratory infection and resolved in about a week. However, about 20% of those infected required hospitalization for pulmonary effects and approximately 2% died. Given global travel, the viral disease, soon to be named COVID-19, spread to Europe and every other country in the world, where it is currently creating absolute havoc. There is no vaccine for this virus nor will there be a vaccine for over a year. There is no effective treatment for COVID-19, no matter what a certain fool at the White House may have said.
The good news is that many areas of the country have put in place many or all of the NPIs that we’ve discussed and these interventions may help to “flatten the curve”. There is also the possibility that as the warmer weather approaches, COVID-19 may begin to disappear as some other respiratory viruses have in the past. Even if both of these happen, this disease will overwhelm our health care system in the next 4 weeks, certainly in NY and possibly in California, Illinois, Florida, and a host of other states.
The US got a late start in answering this call, but now the best we can do is prepare for the worst and hope for the best.
P.S. Have you noticed that the CDC has been totally cut out of any and all communication with the American public on this health issue? The number one epidemiological agency in the world does not communicate directly with the American people on the number one epidemiological issue in the last 100 years. You thinks that’s a good thing?
just read it. Clear and concise. Thanks.
LikeLike
Great read Mike and so accurate of the happenings today
LikeLike